In the News
Antibiotic Resistance Could Be a Top Cause of Death by 2050, Experts Say
Washington,
May 25, 2022
Antibiotic resistance will become a bigger threat over time, experts said during an online panel discussion hosted by The Hill and sponsored by the Pew Charitable Trusts on Tuesday afternoon.
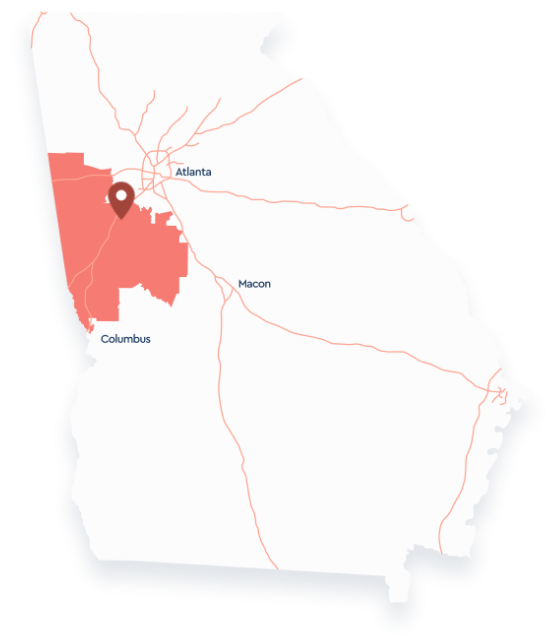
As bacteria evolve, they can render antibiotics useless, which in the U.S. has led to more than 2.8 million resistant infections and over 35,000 deaths each year, according to the CDC. In 2019, more people died from antibiotic resistance than HIV/AIDS or malaria globally. Antibiotic resistance will become a bigger threat over time, experts said during an online panel discussion hosted by The Hill and sponsored by the Pew Charitable Trusts on Tuesday afternoon. As bacteria evolve, they can render antibiotics useless, which in the U.S. has led to more than 2.8 million resistant infections and over 35,000 deaths each year, according to the CDC. In 2019, more people died from antibiotic resistance than HIV/AIDS or malaria globally. One reason this threat has largely gone unnoticed is that, broadly speaking, antibiotics are still effective, noted Sen. Michael Bennet (D-Colo.). "What we have difficulty imagining is what a world looks like where you have an infection and there is no antibiotic and it's widespread," he said. Bacterial infections can occur following common therapies and procedures, from chemotherapy to hip replacements, explained David Hyun, MD, director of the Antibiotic Resistance Project for the Pew Charitable Trusts. "And ... if these antibiotics are no longer able to treat these infections, then we are really undermining all the successes and advances that we have seen across the healthcare setting," he added. Bennet said that he began to take notice of this threat when he read scientists' predictions that antibiotic resistance could become a leading cause of death by 2050, noting that "a complete market failure" to incentivize drug companies to research and develop antibiotics, both in the U.S. and globally, has been one of the key drivers of antibiotic resistance. Kevin Outterson, Esq, executive director of the Combating Antibiotic-Resistant Bacteria Biopharmaceutical Accelerator (CARB-X), a global nonprofit that seeks to hasten the development of antibacterial products that target drug-resistant bacteria, explained that not only does his organization supply companies with grants, "we also support the companies with the technology and experts, so that in 5 or 10 years from now, we're not sitting around wondering why we don't have any antibiotics on the shelf that are available and useful." Dawn O'Connell, Assistant Secretary for Preparedness & Response at HHS, who oversees the Biomedical Advanced Research and Development Authority (BARDA), said that they have been focused on antibiotic resistance for several years, have seen three products come to market, and are currently invested in 18 additional products. Her office has also committed to what's known as the "4-by-30" goal, which involves producing four additional antibiotics by 2030 that would be available for use during future public health emergencies. Antibiotic resistance will become a bigger threat over time, experts said during an online panel discussion hosted by The Hill and sponsored by the Pew Charitable Trusts on Tuesday afternoon. As bacteria evolve, they can render antibiotics useless, which in the U.S. has led to more than 2.8 million resistant infections and over 35,000 deaths each year, according to the CDC. In 2019, more people died from antibiotic resistance than HIV/AIDS or malaria globally. One reason this threat has largely gone unnoticed is that, broadly speaking, antibiotics are still effective, noted Sen. Michael Bennet (D-Colo.). "What we have difficulty imagining is what a world looks like where you have an infection and there is no antibiotic and it's widespread," he said. Bacterial infections can occur following common therapies and procedures, from chemotherapy to hip replacements, explained David Hyun, MD, director of the Antibiotic Resistance Project for the Pew Charitable Trusts. "And ... if these antibiotics are no longer able to treat these infections, then we are really undermining all the successes and advances that we have seen across the healthcare setting," he added. Bennet said that he began to take notice of this threat when he read scientists' predictions that antibiotic resistance could become a leading cause of death by 2050, noting that "a complete market failure" to incentivize drug companies to research and develop antibiotics, both in the U.S. and globally, has been one of the key drivers of antibiotic resistance. It takes 10 to 15 years on average and around $1.3 billion to bring a new antibiotic to market, noted Hyun. "The problem is that the return on investment once those kinds of antibiotics hit those markets is just not there," he added. For that reason, Bennet and a handful of Republican and Democratic lawmakers, including Rep. Drew Ferguson (R-Ga.), reintroduced "the PASTEUR Act," which calls for an $11 billion investment to correct the market failure by incentivizing small drug developers to help restore the antibiotic pipeline. Using a "subscription model," the government would help keep small businesses afloat as they develop antibiotics that might not be used today, but could be vital in the future, Bennet said, adding that another important driver of antibiotic resistance is the overuse and misuse of the drugs. The PASTEUR Act would strengthen current frameworks, including the CDC's National Healthcare Safety Network and their Emerging Infections Program, as well as others that track and report data on antibiotic use and resistance, a press release noted. Kevin Outterson, Esq, executive director of the Combating Antibiotic-Resistant Bacteria Biopharmaceutical Accelerator (CARB-X), a global nonprofit that seeks to hasten the development of antibacterial products that target drug-resistant bacteria, explained that not only does his organization supply companies with grants, "we also support the companies with the technology and experts, so that in 5 or 10 years from now, we're not sitting around wondering why we don't have any antibiotics on the shelf that are available and useful." Dawn O'Connell, Assistant Secretary for Preparedness & Response at HHS, who oversees the Biomedical Advanced Research and Development Authority (BARDA), said that they have been focused on antibiotic resistance for several years, have seen three products come to market, and are currently invested in 18 additional products. Her office has also committed to what's known as the "4-by-30" goal, which involves producing four additional antibiotics by 2030 that would be available for use during future public health emergencies. The U.S. can't fix this problem on it's own, Bennet noted. A global coalition is necessary to ensure countries around the world benefit from the antibiotics that result from current innovations. "This is a global catastrophe waiting to happen, but it's a global opportunity for us to lead," he said.
|
Office Locations
We look forward to meeting with you and developing lasting relationships that can have a major impact on our district and beyond.